Should we be swabbing our noses or our throats for at-home tests? Do rapid tests even detect omicron at all? Are PCR tests the only results we can trust right now?
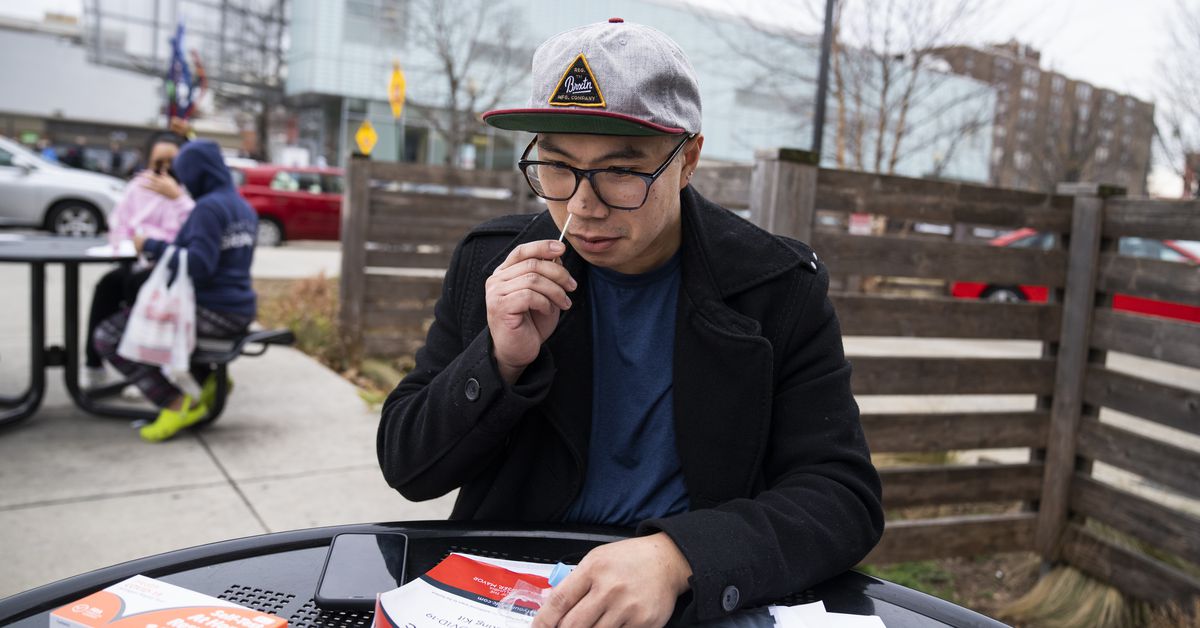
Guidance about how to approach testing in the omicron era seems to be evolving by the day. A recent real-world study that followed 30 subjects likely exposed to omicron found that PCR saliva tests can catch Covid-19 cases three days before rapid antigen tests, which use nasal swabs. These findings, which have not been peer reviewed, follow the Food and Drug Administration’s announcement in late December that, while they do detect omicron, rapid antigen tests may now have “reduced sensitivity.” But that doesn’t mean rapid tests don’t play a key role in our pandemic response going forward.
This is all confusing to a public that’s been pulled in several directions over the course of the pandemic when it comes to guidance and testing. Long delays for PCR test results, a shortage of at-home rapid tests, and the wait for more definitive science about the omicron variant have all made it more difficult to figure out when and how to to get tested. Nevertheless, public health experts say that, as more become available, rapid tests will be an increasingly vital tool for diagnosing Covid-19 and reducing its spread.
So you might be wondering: What’s the point if rapid tests aren’t as accurate as PCR tests? Well, rapid antigen tests, which look for a specific protein on the Covid-19 virus, remain extremely effective at confirming positive cases. Put simply, if you test positive on a rapid test, you almost certainly have Covid-19. If you test negative, in some cases, you might still test positive on a PCR test, which is much more sensitive because it tests for genetic evidence of the virus. Rapid tests may not pick up positive cases in people who have been vaccinated or who have recently recovered from Covid-19, since they may produce less virus, one expert told Recode.
Rapid tests can also reveal a positive case faster than the labs that process PCR tests, since they can take several days to share results with patients, especially during big waves of infection. Perhaps more importantly, rapid tests can indicate whether someone is contagious enough to spread the virus to others, which is what many people are most worried about.
“Given that a rapid antigen test is often the most feasible or available option for many, we don’t want the perfect to be the enemy of the good,” Joshua Michaud, the associate director for global health policy at the Kaiser Family Foundation, told Recode. He explained that every Covid-19 case that’s caught by someone who could take a rapid antigen test but not a PCR test is a win for public health.
Taking rapid tests more frequently also makes them more effective. Most at-home rapid test kits are designed to be conducted over the course of two days, which is why kits typically include two tests. Because each test is a snapshot of the moment it’s taken, multiple tests help reduce the chance of receiving a false negative.
Of course, all of this is assuming that you can get your hands on a rapid test. In the weeks since omicron started to spread, rapid tests have been incredibly hard to find in some parts of the country. These tests are out of stock because neither test manufacturers nor the Biden administration anticipated record levels of Covid-19 cases, which have boosted the demand for rapid tests. To confront the shortage, the White House plans to buy and distribute 500 million free rapid tests in the coming weeks. When that happens, these tests could help catch more positive cases and lower the number of people infected with Covid-19.
The accuracy of a rapid test depends on how often you’re testing yourself and whether you want to identify a Covid-19 infection or measure your contagiousness. But if you test positive on a rapid test, you should trust the result, assume you’re infectious, and isolate for at least five days. If you test positive again after five days, the CDC recommends isolating for five more.
Rapid tests, however, are not perfect. Research indicates that antigen tests are less accurate than PCR tests — this has been the case since the beginning of the pandemic. PCR tests are processed in a lab, where sophisticated equipment can identify and amplify even the tiniest genetic evidence of the virus that causes Covid-19. These tests are so precise that patients can actually test positive for weeks after they’ve recovered and are no longer contagious. The results of rapid tests, meanwhile, can vary based on how much virus is in a patient’s nose at the time the sample is taken and how far along they are in their infection.
Scientists explain the difference between rapid tests and PCR tests in two ways: specificity, which reflects a test’s false-positive rate, and sensitivity, which reflects a test’s false-negative rate. Both PCR and rapid tests have high specificity, which means that their positive results are very trustworthy. But while PCR tests tend to have near-perfect sensitivity, rapid antigen tests tend to have a sensitivity around 80 to 90 percent. This means that rapid tests tend to produce more false negatives than PCR tests do.
Omicron makes testing even trickier. The sensitivity of rapid tests may be even lower for omicron cases, according to early research from the FDA and other scientists. Another problem is that omicron may propagate more in the throat than the lungs, and it could take longer for Covid-19 to show up in nasal samples, even if someone is symptomatic. It’s possible that vaccinated people and people who have recently recovered from Covid-19 are noticing more false positives on rapid tends because they tend to produce less virus overall.
“At-home tests are mostly effective when the person has high viral loads, a time when the person is more likely to transmit the virus,” Pablo Penaloza-MacMaster, a viral immunologist at Northwestern’s medical school, told Recode, “Most at-home tests are still able to detect infection by omicron because they target a part of the virus that doesn’t mutate that much.”
Separate studies from both the UK’s Health Security Agency and researchers in Australia found that antigen tests are as sensitive to the omicron variant as they were to earlier strains of Covid-19. Again, the FDA does still recommend rapid tests to diagnose positive cases, and test manufacturers say they’re confident in their products’ ability to detect omicron. While early research indicates saliva tests might detect Covid-19 more quickly, right now most of the PCR tests and all of the available rapid at-home tests that have emergency use authorizations from the FDA use nasal samples.
Which brings us back to the question of whether you should be sticking nasal swabs in your throat. There is evidence that saliva samples may be a quicker indicator of Covid-19 cases, but that doesn’t mean you should stop following the directions that come with your test kit. The FDA says that people should not use rapid antigen tests to swab their own mouths. Some experts say you might consider doing so anyway, and point out that other countries, including the UK, have approved rapid antigen tests that use throat swabs and released very careful directions about how to do so.
“I personally do swab my throat and my nose to get the best sensitivity when I use over-the-counter tests at home,” Michael Mina, an epidemiologist at Harvard, said at a Thursday press conference. “There are risks associated with that, but the biology does tell us that they might be getting better sensitivity earlier.”
But the concern with rapid test kits right now is not that people are swabbing their noses, but how often they’re swabbing their noses. A single test could miss a Covid-19 case and produce a false negative, but taking two tests over a 24 to 36 hour period reduces this risk. The more rapid tests you take, the more you reduce your chances of a false negative, and the more times you test negative over multiple days, the more confident you can be that you’re not spreading Covid-19.
Still, the biggest problem right now is that rapid tests are pricey and hard to find. Pharmacies have limited the number of test kits people can buy, and many are completely sold out. A single test can also cost more than $10, which means that testing yourself regularly gets expensive quickly. Opportunists have even hoarded tests and engaged in price gouging, which has exacerbated the shortage.
If you don’t have enough tests to test yourself regularly, it’s best to test yourself right before seeing vulnerable people, says Mara Aspinall, a professor who leads Arizona State’s testing diagnostic commons and a board member for the test manufacturer Orasure, told Recode. “I’m heading to a vulnerable person [or] I’m going into a health care setting, and therefore need to test right beforehand.”
For now, the best test kit is the test you can get (Wired has a handy list of the brands currently available). If you’re planning to go somewhere and don’t want to spread the virus, you should take one rapid test the day before traveling, and then a second test immediately before you go. If you only have one rapid test, take it right before you see people.
Testing yourself should become easier as more rapid tests become available. In addition to the 500 million free rapid tests that the White House will distribute beginning later this month, people with private insurance will also be able to get their rapid test purchases reimbursed starting next week. You should also check with your local health department, as they might be distributing free tests.
Even though the rapid test situation is still less than ideal, there are other strategies we can use to protect both ourselves and other people from Covid-19, like getting vaccinated, getting boosted, and wearing a mask. And if you do happen to find some rapid tests, go ahead and grab them. They might just come in handy, especially if you use them correctly.
source https://www.vox.com/recode/22870328/how-to-use-rapid-tests-omicron

Post a Comment